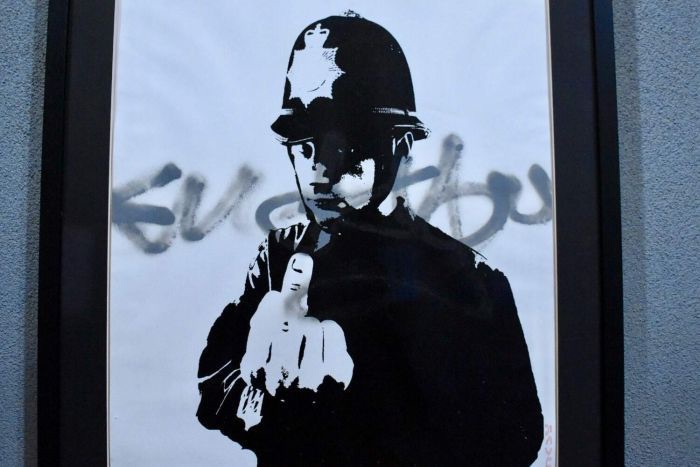
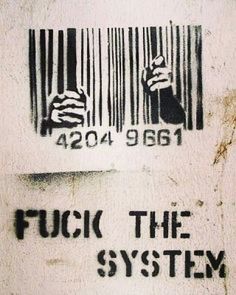
New Study says Black Men & White Men Have the Same Risk of Dying from Prostate Cancer When Access to Care and Treatment are Equal: Disparity is Due to Racism/White Supremacy Not Genetics
/White Over Black System of Vast Unequal Power & Conditions From [NBC] For African American men, the risk of dying from prostate cancer is the same as that of white men when access to care and treatment are equal, a new study finds.
This casts doubt on the widely held belief that, when it comes to African American prostate health, genetic factors play a larger role than health disparities.
The results of the study were published Thursday in the journal JAMA Oncology.
“Black men have similar outcomes to white men once they’re diagnosed with prostate cancer, when you account for differences in access to health care and receiving guideline-recommended treatment,” said lead study author Dr. Daniel Spratt, associate professor and vice chair of radiation oncology at the University of Michigan. “In fact, black men, on average, had better outcomes than white men, when looking at patients who enrolled on clinical trials.”
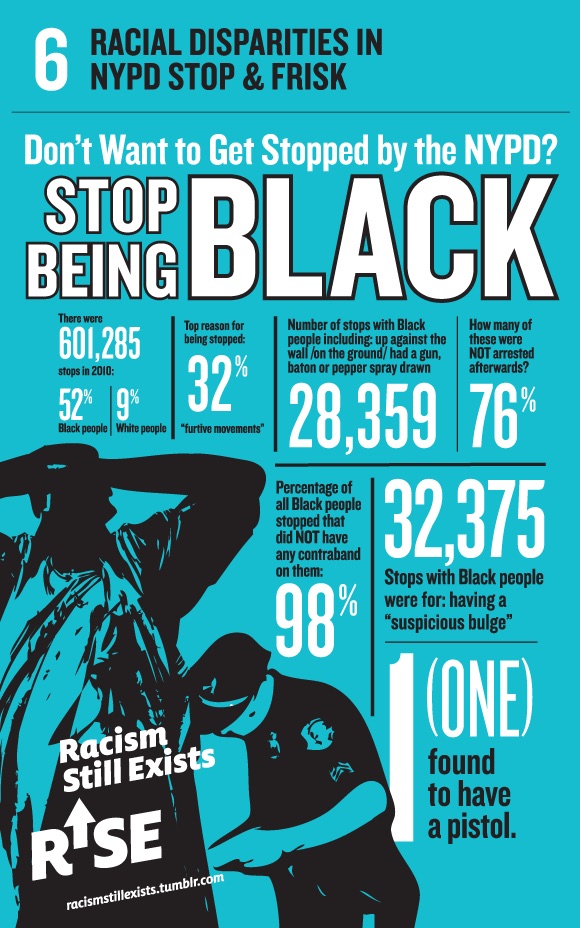
“This data suggests that — although on the population level, more black men die from prostate cancer than white men — this disparity is largely, if not entirely, driven by social constructs and even systematic racial disparities in our country,” Spratt told NBC News. These include less access to health care, insurance, and appropriate and timely treatment.
The University of Michigan researchers led by Spratt and Dr. Robert Dess looked at data from 306,100 men — 54,840 black men — ages 59 to 71 from the Veterans Affairs system and four other clinical trials. When the researchers compared black and white men of similar age, socioeconomic status, and tumor characteristics, such as prostate specific antigen (PSA) levels, stage and grade of cancer — all of which predict the cancer’s aggressiveness — they found that black men had comparable rates of death to white men, when they had similar access to care and standardized treatment.
The new findings underscore the need for equal access to care and treatment.
“When a black man shows up in my clinic [for prostate cancer treatment], I am confident that I can tell him that he will have very similar long-term outcomes … to a white man, in regards to dying of prostate cancer,” Spratt said.
“This study debunks that there is a large genetic driver of stage-for-stage worse prostate cancer outcomes in black men compared [with] white men, and [instead suggests] that previously detected differences are largely, if not entirely, driven by social and cultural factors.”
Socioeconomic factors, for example, could play a role in the disparities seen between black and white men with prostate cancer, said study co-author Dr. Brandon Mahal, a radiation oncologist at Dana-Farber/Brigham and Women’s Cancer Center in Boston who researches prostate cancer.
But another factor, Mahal said, is that doctors may provide biased treatment to black men, based on the idea that they inherently have more aggressive cancers.
Mahal published a separate study Wednesday in the New England Journal of Medicine that looked at the increasing trend of conservative management for low-risk prostate cancer. That study noted that, while conservative management for prostate cancer has increased for both black and white men, doctors offer the approach to black men disproportionately less often than white men.
“Conservative management of low-risk prostate cancer — through either active surveillance or watchful waiting — has been increasingly used as an alternative to radiation … or [surgery]. However, this approach may be underused among black men, because they are generally underrepresented in clinical trials and are thought to have more aggressive cancers,” Mahal said.
A larger conversation on health disparities
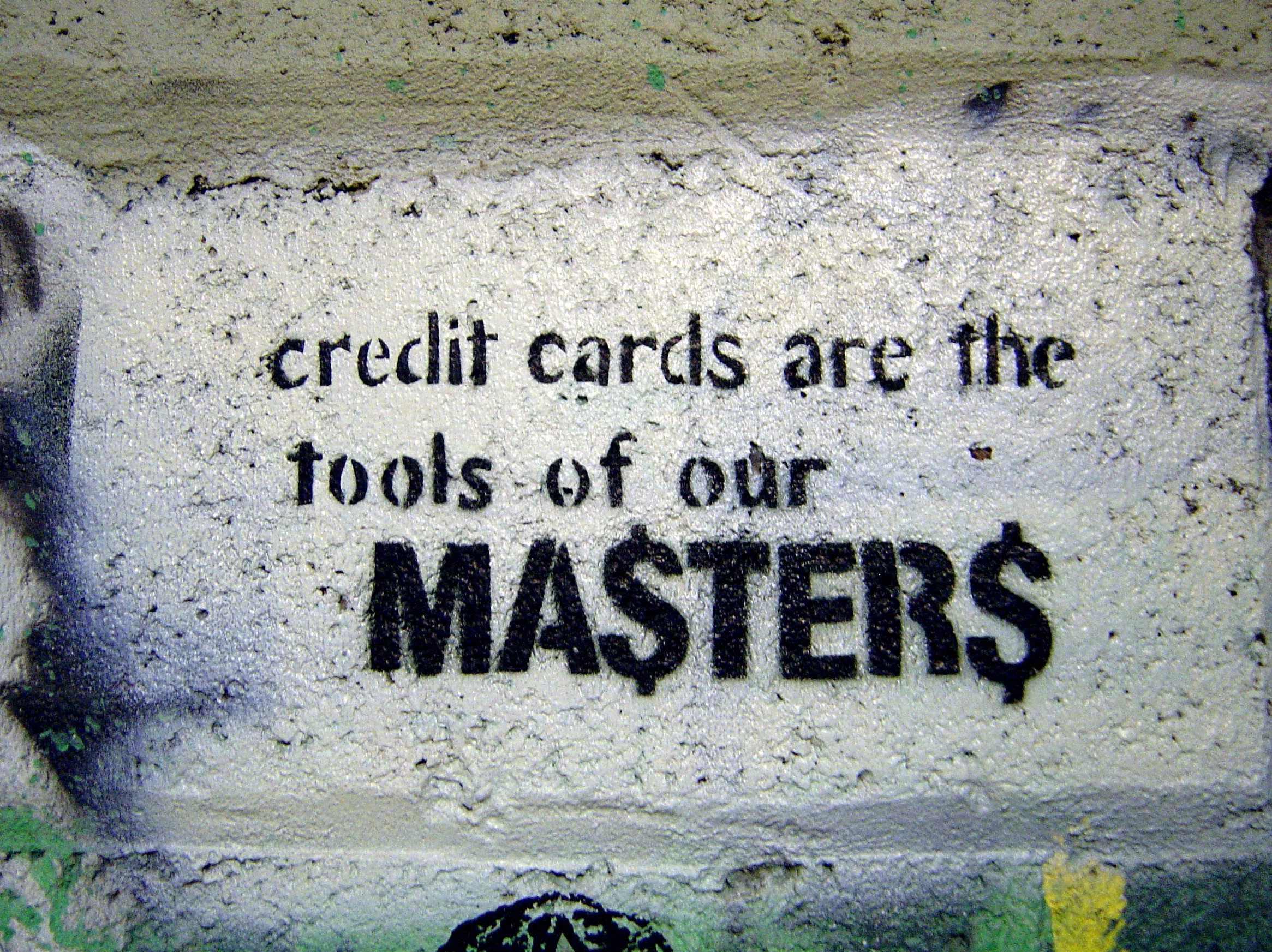
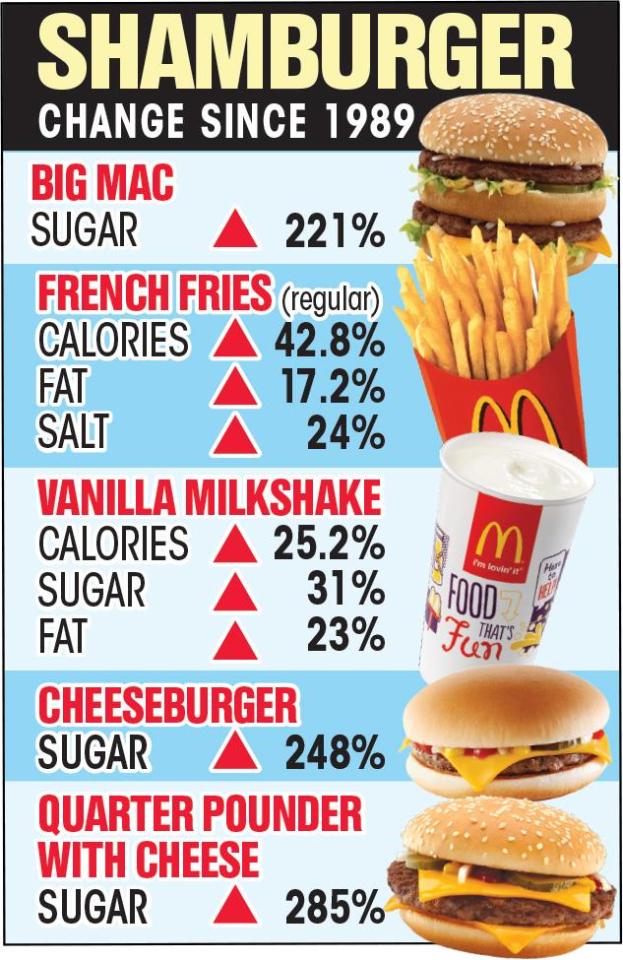
Factors leading to health disparities for prostate cancer in African Americans include stress, income, lifestyle and poor diet. Biological differences and medical access also contribute.
Prostate cancer is diagnosed in about 164,000 American men every year. It kills about 29,000 a year, according to the American Cancer Society. And African American men have about a 15 percent chance of developing prostate cancer in their lifetimes, compared to about a 10 percent chance for white men, according to the National Institutes of Health.
Previous studies — most notably the SEER trial — have shown that African American men have the highest rates of new prostate cancer diagnoses (158.3 per 100,000 men) and are twice as likely to die from the disease as white men. Although this disparity is nothing new, researchers have been unable to provide concrete answers as to why it exists.
While the new JAMA Oncology study does not answer the question of why black men develop prostate cancer more often than white men, it does highlight several factors that black men should be aware of when addressing their health.
Compared with white men, “black men have lower rates of PSA screening, are often diagnosed at [a] later stage of disease, have less access to insurance, have lower socioeconomic status, and higher rates of obesity and diabetes … all of these factors impact the type of treatment they receive and their ability to complete” that treatment, Spratt said. “These differences likely largely explain why, on a population level, black men are more likely to die from prostate cancer than white men.”
More importantly, Spratt notes that the numbers of black men dying from prostate cancer pale in comparison to the numbers of black men dying from causes such as heart disease. But this research opens the door to a larger conversation.
“The larger and more important question to address is why black men are dying [at higher rates than white men] of other causes, like heart disease. This emphasizes the importance of addressing the social inequities for black men [in the U.S.] and making sure they have access to, and can afford timely and quality health care,” Spratt said.
Spratt and Mahal both believe that increasing racial diversity in clinical trials, as well as in the health care workforce, can go a long way in helping to create true equality in health care.
“America needs fundamental socioculture changes to reduce — and hopefully one day eliminate —discrimination, and [to] improve access to health care, providing insurance coverage and … access to quality care not just for cancer, but for other diseases” as well, Spratt said. “One method that can help with this is by expanding the diversity of the health care workforce.”